Winning the battle against antimicrobic-resistant bacteria – new technology allows our healthcare to respond to a rising threat
Share
WHO 2022 World Antimicrobial Awareness Week 18 - 24 November 2022 - GO BLUE (see the WHO theme site)
- European Center for Disease Control (ECDC, 2018)
The World Health Organization (WHO) has declared that antimicrobial resistance (AMR), and especially the development of antibiotic resistant bacteria, is one of the top 10 global public health threats facing humanity [1].
In the worst scenarios, the development of antimicrobic-resistant bacteria can cancel out the advancements in modern medicine, making today’s common medical procedures lethal and treatable diseases uncurable tomorrow. The cost to our societies could be far worse than the Coronavirus pandemic has caused.
Coordinated cooperation between different sectors of human activity, from food production to healthcare, as well as the adoption of new innovative technologies are needed to prevent the looming catastrophe. The good news and source of hope is that the awareness, will to act, and field-proven technology are all available. But we must react now.
In this article we show what we all can do to fight antibiotics resistance. We are also giving you an informed update on the situation.

What is antibiotics- and antimicrobics resistance and how it affects our healthcare?
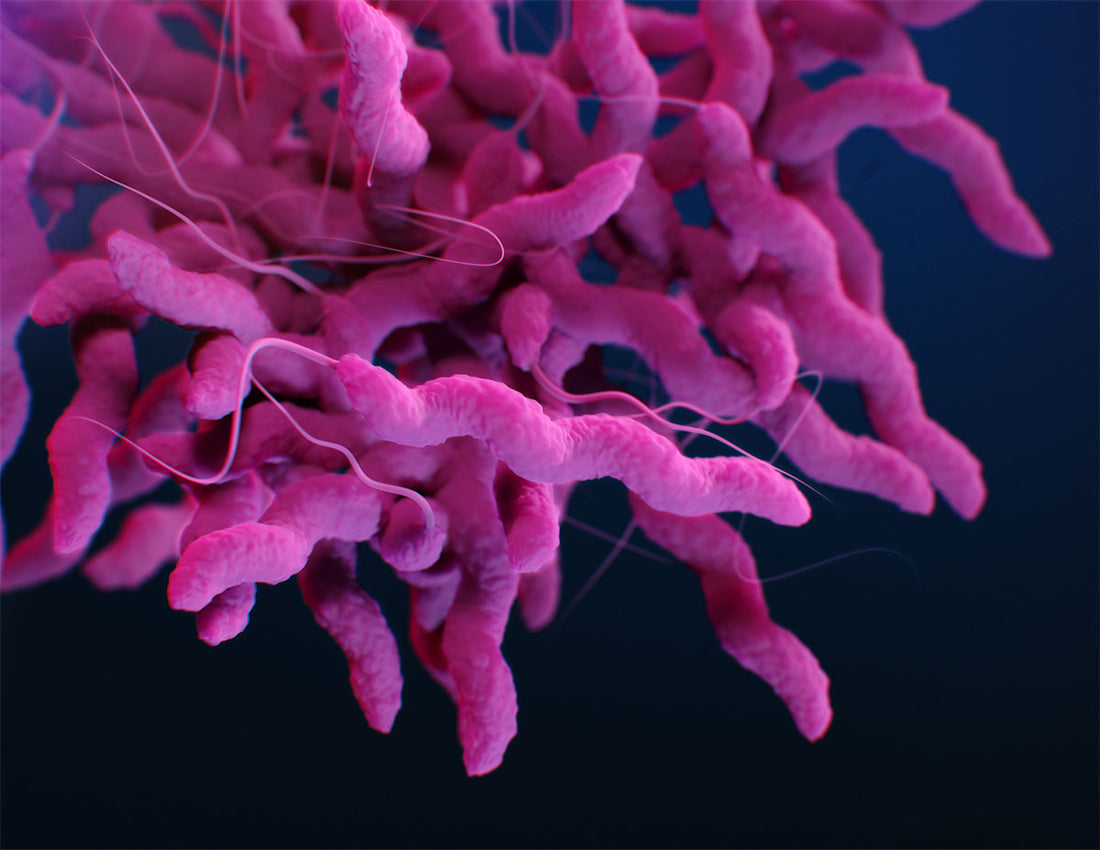
Antibiotics are medicines used to prevent and treat bacterial infections. Antibiotic resistance occurs when bacteria change in response to the use or misuse of these medicines, developing immunity to them. Antimicrobics are all kinds of substances used to kill microbes. Antibiotics are one type of antimicrobics, chemical disinfectants are another type of antimicrobics. Multi-resistant strains have developed resistance to more than one antibiotic, and can often have developed resistance to several chemical disinfectants as well. These are often in media called “superbugs”, and are becoming more common in health care settings.
Typically, antibiotics (and other antimicrobials, most chemical disinfectants and ultraviolet light) have only one mechanism how they influence the target microbe, preventing its growth, reproduction or damaging its vital functions. When the antimicrobial treatment fails to defeat the bacterial colonies completely, any viable bacteria left behind may respond by developing defenses against the used mechanism. If one bacterium has developed a defense, it can transfer the defense mechanism to other bacteria, spreading the resistance.
The misuse and overuse of antibiotics are driving the fast development of drug-resistant strains of bacteria and making them more and more widespread in hospitals and health care setting, in poor countries and rich countries alike. Already today, according to ECDC, 1 in 3 healthcare-associated infections (HAI) in European acute care hospitals and long-term care facilities are caused by antibiotic-resistant bacteria [2.].
The most common bacteria found in European hospitals in 2019 are E. coli (44.2%), followed by S. aureus (20.6%), K. pneumoniae (11.3%), E. faecalis (6.8%), P. aeruginosa (5.6%), S. pneumoniae (5.3%), E. faecium (4.5%) and Acinetobacter species (1.7%) [3]. Among these are found strains already known to have developed resistance to common antibiotics and causing problems in healthcare are for example methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), multi-drug-resistant Mycobacterium tuberculosis (MDR-TB) and carbapenem-resistant Enterobacteriaceae (CRE) gut bacteria. MRSA has been causing problems for quite some time, recent statistics from 2019 shows an increase in especially VRE in European hospitals [3].
When infections can no longer be treated by commonly available antibiotics, more expensive treatments must be found and used. Our healthcare capacity will be stretched to and beyond its limits when treating patients requires more and more time and medication.
- WHO
How visible blue light helps healthcare organizations prevent antimicrobic-resistant bacteria in their environment
- A modern, touch-free, chemical-free and UV-free disinfection method for surfaces and air.
- 100% safe for people and materials, can be used for continuous disinfection even in occupied rooms.
- Works against all bacteria, including antibiotic-resistant strains, molds and yeasts.
- Does not promote antimicrobial resistance.
- Works against SARS-CoV-2 and influenza A viruses.
- Already in use in operating rooms and ambulances in Europe and USA.
- Perfected and patented by LED Tailor Oy (Finland).
Antimicrobic resistance is a complex problem that requires the design and implementation of new coordinated policies and procedures, as well as the adoption of new technologies that can help us reduce the use of antimicrobials such as antibiotics and chemical disinfectants.
In the healthcare sector, to prevent and control the spread of antibiotic resistance, WHO’s first recommendation to healthcare professionals is to make sure that the environment is clean, including surfaces, equipment and hand hygiene.
Our recommended approach for hospitals is to use suitable detergents to clean the facilities daily, removing soil and dirt, and to deploy automatic and continuous visible blue light disinfection to eliminate any remaining pathogens on hospital surfaces and air.
Blue light photon disinfection is a novel technology that uses safe, visible wavelengths of blue light (no UV light) to kill microbes in air and on surfaces. Its efficacy has been shown in over 2000 peer-reviewed articles (PubMed, 2021) and it is already being successfully used in operating rooms and ambulances to ensure a high hygienic level [4,5].
Visible blue light has been shown to effectively eliminate and prevent the growth of all bacteria, including multi-resistant strains (e.g. MRSA and VRE). The mechanism how visible blue light inactivates bacteria is through creation of reactive oxygen species (ROS) inside the bacterial cell. The ROS cause a large variety of damage to all internal cell structures, making it practically impossible for the bacteria to repair and develop resistance.
Using blue light in operating rooms has already been shown to reduce surgical-site infections by 75% [4].
The technology is available and ready, and requires no new procedures or training for the staff. It makes perfect sense to deploy it now, when there is still time.
More infomation:
Kirsi Saukkonen, Senior Specialist, Infectious Diseases.
LED Tailor Oy
kirsi.saukkonen@ledtailor.fi
References:
1. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
2. European Centre for Disease Prevention and Control, 2018. Infographic: Healthcare-associated infections – a threat to patient safety in Europe. (https://www.ecdc.europa.eu/en/publications-data/infographic-healthcare-associated-infections-threat-patient-safety-europe)
3. European Centre for Disease Prevention and Control. Antimicrobial resistance in the EU/EEA (EARS-Net) - Annual Epidemiological Report 2019. Stockholm: ECDC; 2020.
4. Murrell LJ, Hamilton EK, Johnson HB, Spencer M. Influence of a visible-light continuous environmental disinfection system on microbial contamination and surgical site infections in an orthopedic operating room. Am J Infect Control. 2019 Jul;47(7):804-810. https://doi.org/10.1016/j.ajic.2018.12.002
5. https://www.profilevehicles.com/en/automatic-disinfection-of-ambulances-with-blue-light/
