Blue Light Eliminates Microbial Biofilm Effectively
Share
Research shows that antimicrobial blue light (aBL) can penetrate biofilm and eliminate microbes inside it effectively (McKenzie et al, 2008, Wang et al. 2016). This blog article explains why Spectral Blue is especially useful in disinfecting biofilms. We also give further background information on biofilm and how it can affect pharmaceutical and medical device manufacturers and healthcare operators.
“Research shows that blue light, unlike common biocides and UVC radiation, is very effective against bacteria inside biofilm.”
Biofilms are known for being extremely resistant to traditional antimicrobials. Chemical disinfection of biofilms requires stronger concentrations, longer contact times and more mechanical effort to work. With UVC radiation the doses required for disinfecting biofilm are much higher than normally, leading to illumination times that are unfeasible in areas where there are people working and delicate laboratory or healthcare equipment is used.
Researchers have tested antimicrobial blue light in the range of 405 to 470 nanometres against a multitude of biofilm forming microbes, both with single-species and multi-species biofilms. While the intensities and dosages have varied across studies, the conclusion is that blue light kills microbes inside a biofilm effectively.
The three factors that make Spectral Blue a great weapon against biofilm are:
- Blue light penetrates biofilm better than most chemicals and UVC. It can reach the microbes behind the protective layer and affect them directly. Additionally, when biofilm grows on transparent surfaces such as glass and plastics, like pipettes or other laboratory kit, blue light can reach it from both sides - UVC and chemicals cannot do this.
- Blue light is very unlikely to promote the development of antimicrobial resistance. The mechanism of action of Spectral Blue is based on activating light-absorbing compounds and generating reactive oxygen species inside the microbial cells. The ROS cause wide-ranging and unspecific damages, which make it very difficult for the microbes to develop resistance. Chemicals and UVC typically have only one mechanism of action, which make it easier for microbes to develop resistance against them.
- Blue light can be safely used continuously. While blue light energy doses required to kill microbes in biofilm form are higher than with non-biofilm forms, you can use Spectral Blue throughout the day without risking people or equipment. This allows you to gradually eliminate the biofilms on surfaces and then keep them from forming again. UVC and chemicals can only be used periodically, allowing microbes to grow freely for most of the day.
What is a biofilm
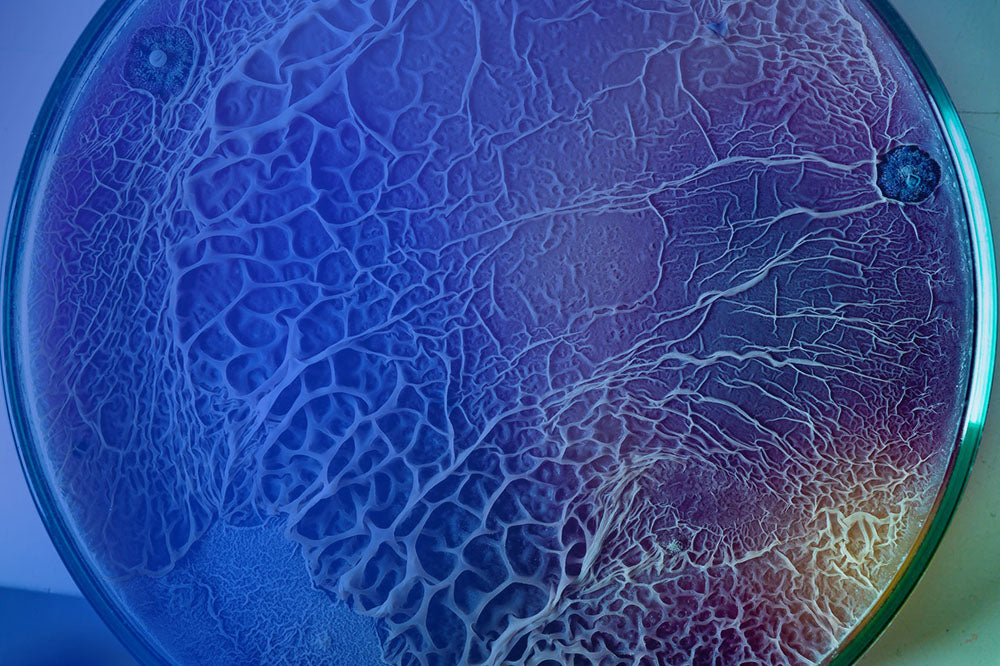
Biofilm is a living system that is formed by one or several groups of micro-organisms adhering to each other and often to a solid surface. It provides protection from the environment and allows the microbes to reproduce quickly. Biofilms can be formed by a single kind of microorganism, but typically they are complex mixtures of several species of bacteria, fungi, yeasts, and other microorganisms (so called polymicrobial biofilms).
Moisture and availability of nutrients typically promote the formation of biofilm. Biofilms can form on all kinds of surfaces, for example metals, plastics, kitchen counters, medical devices and implants, water tanks, pipes, swimming pools, and human tissue. One example of biofilm is the plaque that forms on teeth. Biofilm can be invisible, just a couple of cells thick structure, or it can grow to form very visible structures of slimy goo that can even block drainpipes.
Read here in more detail about the most common sources of microbial contamination in cleanrooms.
Biofilms are a significant problem for healthcare and cleanroom industries. It is estimated that 65-80% of all infections are caused by microbes in biofilm form. Polymicrobial biofilms can also promote antibiotic resistance by allowing interspecies transfer of antibiotic resistance genes (Ferrer-Espada et. al, 2019). Biofilms are estimated to be responsible for more than 65% of nosocomial infections, approximately 80% of chronic infections, and 60% of all human bacterial infections (Assefa & Amare, 2022).
“Biofilms are estimated to be responsible for more than 65% of nosocomial infections, approximately 80% of chronic infections, and 60% of all human bacterial infections.”
Some well-known examples of biofilm forming bacteria are Enterococcus faecalis, Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis and Pseudomonas aeruginosa.
How does a biofilm form?
Biofilm formation is usually divided into phases. First, the microbes attach themselves to a surface. Once attached, they start creating a protective layer by secreting mucous substances. Having created the layer, the colonies gradually mature to the point where they are able to start dispersing and creating new biofilms on neighbouring surfaces.

Biofilm formation is a cyclical process, where cycles of maturation and expansion repeat. It is also a quick process, as the early phases of attachment and biofilm formation can take place within minutes. This speed of dispersion makes preventing biofilm formation a daunting task. Furthermore, every biofilm is unique; a single biofilm can contain even hundreds of different species of microorganisms.
Why disinfecting biofilms is difficult?
Biofilms make the microbial colonies inside highly resistant to environmental stressors. This makes eliminating them without mechanical action very difficult.
The outer layer of the biofilm constitutes a strong physical protection against disinfecting agents. Usually very high concentrations of chemical disinfectants are needed in comparison to routine disinfection. For example, removing biofilm with chlorine requires a concentration of ca. 30 000 ppm, while routine disinfection requires a concentration of ca. 500-1000 ppm.
Eliminating biofilms with chemical disinfectants also requires longer contact times and more intense mechanical action to work.
Ultraviolet radiation and hydrogen peroxide gas, the most common automatics disinfection tools, cannot remove biofilm. UVC radiation has a relatively low ability to penetrate materials. It can only affect the outermost part of the biofilm.
Spectral Blue disinfection system and biofilms
Antimicrobial blue light has been shown to be effective on biofilm-based microbes. Visible blue light is able to penetrate different materials, including biofilms, and eliminate microorganisms inside them. This makes The Spectral Blue disinfection system significantly more effective on biofilm than the competing automatic disinfection techniques.
The Spectral Blue disinfection system can be used to reduce dependency on manual processes. In continuous use it can reduce biofilm formation and eliminate already formed films.
The Spectral Blue disinfection system uses Multi-Wavelength, High-Intensity (MWHI) blue light, combining the most efficient antimicrobial wavelengths at 405 and 430-470 nanometre bands at high intensity. This allows the system to eliminate a broad range of different microorganisms and with less energy than traditional single-wavelength blue light systems.
Read more about the science behind Spectral Blue disinfection system here.
References and further reading on the topic:
McKenzie K, Maclean M, Timoshkin I V, Endarko E, MacGregor S J, Anderson J G. Photoinactivation of bacteria attached to glass and acrylic surfaces by 405 nm light: potential application for biofilm decontamination. Photochem Photobiol. 2013 Jul-Aug;89(4):927-35. URL: https://pubmed.ncbi.nlm.nih.gov/23550978/
Assefa M, Amare A. Biofilm-Associated Multi-Drug Resistance in Hospital-Acquired Infections: A Review. Infect Drug Resist. 2022 Aug 31;15:5061-5068. doi: 10.2147/IDR.S379502. PMID: 36068834; PMCID: PMC9441148. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9441148/#cit0004
Ferrer-Espada R, Liu X, Goh X, Dai T. Antimicrobial Blue Light Inactivation of Polymicrobial Biofilms. Front Microbiol. 2019 Apr 9;10:721. doi: 10.3389/fmicb.2019.00721. PMID: 31024499; PMCID: PMC6467927. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6467927/
Coenye T, Biofilms, Brenner's Encyclopedia of Genetics (Second Edition), Academic Press, 2013, Pages 335-337, ISBN 9780080961569, https://doi.org/10.1016/B978-0-12-374984-0.00154-6.
Wang Y, Wu X, Chen J, Amin R, Lu M, Bhayana B, Zhao J, Murray C, Hamblin M, Hooper D, Dai T, Antimicrobial Blue Light Inactivation of Gram-Negative Pathogens in Biofilms: In Vitro and In Vivo Studies, The Journal of Infectious Diseases, Volume 213, Issue 9, 1 May 2016, Pages 1380–1387, https://doi.org/10.1093/infdis/jiw070

